Types of leukemia
Leukemia is a type of blood cancer that usually originates in bone marrow. Although it is the most common type of cancer in children, most cases of leukemia develop in adulthood. The common characteristic of leukemia is a high number of aberrant cells present in the blood. These cells are partially differentiated precursor blood cells with altered gene expression and the presence of specific plasma membrane markers. Leukemia is classified based on the type of aberrant cells found in patients. They can originate from lymphoid (lymphocytic leukemia) or myeloid (myeloid or myelogenous leukemia) lineage. Leukemia is then further divided into acute and chronic, depending on the disease progression. Investigating markers of the aberrant cells is indispensable for correct diagnosis and subclassification (immunofluorescence, immunohistochemistry, and flow cytometry), monitoring the disease progression, and the further development of therapeutic treatments.
Lymphocytic leukemia
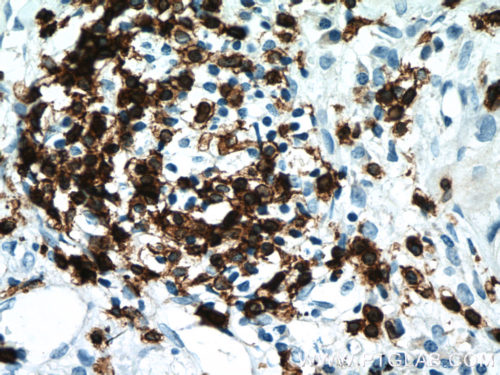
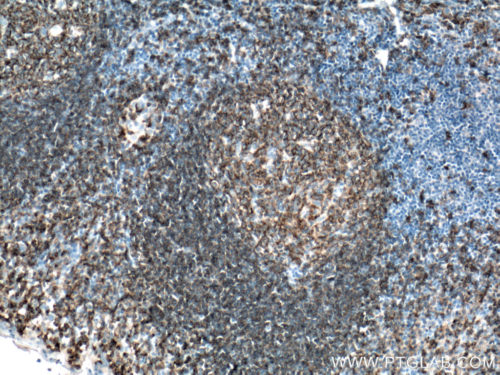
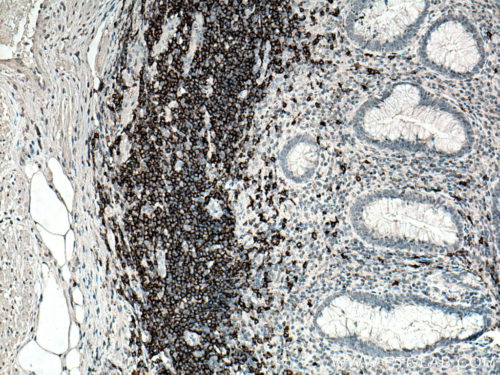
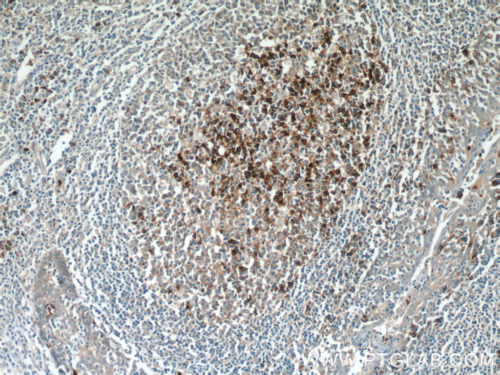
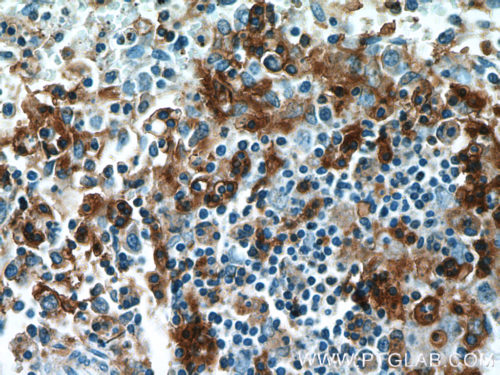
The two main types of lymphocytic leukemia are chronic lymphocytic (CLL) and acute lymphocytic (ALL). Patients have elevated levels of lymphoblasts (precursors of white cells) in their blood. These can be either T or B cell lineage. CD3 (Figure 1), CD4, and CD8, as classic markers of T cells, are a good prognostic marker of patient survival (PMID: 20846097). CD19 (Figure 2), an antigen widely present on B cells, persists in its expression on B cell-related cancer cells. It is often used in diagnosis (PMID: 8528044). Additional markers, namely CD20 (Figure 3), CD22, CD24, and CD79a, are used to study minimal residual disease – drug-resistant leukemic cells (PMID: 9492773). Plasma membrane staining of CD38 (Figure 4) and CD49d is often used in the clinic and their expression correlates with the disease severity and its response to chemotherapy (PMID: 10477712). ZAP70, an intracellular protein, is also a predictor of leukemia. It is involved in promoting prolonged signaling of the BCR pathway and the survival of cancer cells (PMID: 18577710).